Sometimes, words aren’t enough.
We are doing our best. Love, let it be enough. For today, at least.
Living and loving life (most days), despite SNUC (Sinonasal Undifferentiated Carcinoma)
Sometimes, words aren’t enough.
We are doing our best. Love, let it be enough. For today, at least.




Home again home again, jiggity jig.
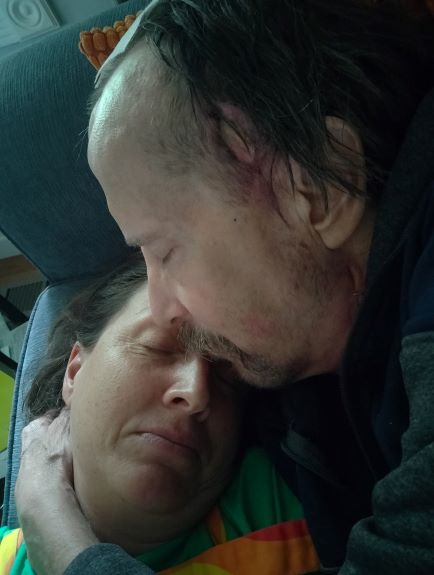
Mark in his happy place. Me too.
Both of my children are trans. They are adults, not children. They are 23 and 24. Their stories are their own, and they are unique. My heart is wrapped tightly around each of them. I remember with one of them, when they told me, and then told me again, and then desperately tried again to explain to me … finally something made sense. I was going to go there with them, or I would be sending them off into a life I would never truly know, with a wound slashed so deep that it would stretch from me to them. “I don’t know where you are going, but I’m going there with you,” I remember saying. It may have been my greatest leap of faith, ever. When you have a trans kid, or two trans kids, you have your skin peeled back and then you grow a thicker one. The old skin is the expectations that culture puts on you, your upbringing puts on you. Subconscious. Friends. Family. Religion. Workplace. Gender identities that slip past the narrow boundaries our society allows are deeply threatening to many. Surprising. Confusing. The new skin you grow is understanding. Empathy. A love with a fierceness great and wide. When your kid comes to you and says, this is me, please see me, the choice is clear. You rise or you fall. Too many parents fall. You? You see them. And you hold on tight as they carry you to places you’ve never been.
I feel this way, on the eve of bringing home a wheelchair with Mark in it. I have only one choice. It’s to go with him. He is there. I would imagine that he is just as scared as I am.
I could rise or I could fall.
Me? I am rising.
I will give it my all.

Today. The occupational therapist trained me in wheelchair transfers from bed to chair, wheelchair to toilet, wheelchair to shower chair. Tomorrow, the physical therapist will teach me how to help Mark with steps. The patient care technician, changing Mark’s bed linens, said, “It’s exciting that he’s going home so soon.” “Well, to him,” I replied. My actually mood? This photo.
I’m deep into purchasing solutions. Makes me feel like I’m doing something. More grab bars. A shower chair with a back and arm rails. Shower wands for the two possible bathroom showers he might use. An alarmed mat to put next to his side of the bed so I can sleep without the terror of not waking up when he tries to get onto the bedside commode. A bed railing to help him get up safely. A bell he can ring if he needs something.
Someone just offered me a portable ramp, so Mark will be able to get out onto the patio and sit in the sun. Someone offered to help teach Matthew to drive, which I sadly must pass on to another adult as I can not be sure I could do it anymore.
I am many phone calls into looking for caregivers. I’ve tried to create an elevator pitch out of a story that is a long and tragic novel. It’s hard to summarize. I’ve struck out with agencies but have found a couple women who may be able to come in next week for parts of a few days. I’ve talked to the boys and told them how their dad he will look. How he can and cannot move. The new level of supervision he will need. That I will train them in how to do this when it is inevitably their turn. That today he kept asking me where his keys were. “But how will I get the car out of the [hospital] garage?” He asked over and over, no matter how I responded. Listening, answering, redirection, distraction, diversion. The options available.
I am on high, high alert. Poised for the storm. Trying to prepare. Batten down the hatches. Prepare the fallout shelter. Breathe. Breathe. Breathe.
I can’t come up with a title for this post. I found out today that Mark is being discharged with a loaner wheelchair, and a permanent wheelchair will arrive in a couple months. Will he ever walk again unassisted? Maybe. The therapists don’t know. For now, the one remaining muscle that attaches his quad to his knee is not firing. He can walk for about two minutes, tops, before the knee gives out. He cannot walk safely, at all, without a person right next to him to catch him in case he falls. He only needs assistance when walking, not when sitting, but with his frontal lobe injury, he impulsively decides it’s time to get up and do something. He still has a 24/7 one-on-one aid in his room, watching him. When he comes home, that job will be mine and the kids.
When he went into surgery, my greatest fear was that he’d have a stroke. That he’d come out with a greater level of need. I thought we dodged that bullet. We did not.
Tonight, I removed the living room area rug. I rearranged the living room furniture, the kitchen table. I removed Mark’s dining room chair. Our wonderful neighbor, Rob, is here installing grab bars for the toilet and a child-proof gate for the top of the steps so Mark doesn’t accidentally tumble down.
Mark is coming home on Friday.
In a wheelchair.
I am trying to figure out how to get him safely into the house.
I can’t believe it.
I’m not prepared.
Here’s how I felt today, when I heard it:
I.
Give.
Up.
Mark will likely be discharged on Friday. He’s making progress in many ways. He’s compliantly working with PT, OT and speech six days a week. He’s still refusing his heparin shot and bloodwork, so his need to stand his ground in order to feel he has some control over his life is intact. At least he’s accepting his other medications. His mood has leveled out quite a bit, thankfully. In some ways, the parts of this post-treatment phase that are about frontal lobe injury are familiar to me. I’ve navigated from where he is now up to a better baseline before. So while I did burst into tears when the case worker told me they were preparing him for discharge, I do know that I can adjust to having this version of Mark home again. In this case, being familiar with it is not necessarily a positive. The tears were because I know, from experience, that it will be a lot. For me and for the boys. The tears were also because Mark cannot walk unassisted, period. The reason for this is surgical. There’s two muscles, I have learned, that connect your quads to your knee. One of those is where it belongs. The other is now living in Mark’s forehead. His knee now buckles when he walks, and it does so unpredictably. Will his other muscles figure out how to compensate? I have no idea. So for Mark to get up every morning, for him to get to the couch, for him to get to the dining room table for meals, for him to get to the bathroom, will require a person holding onto him. This is a new level of … well, I don’t know the right words for it. I’m too tired to come up with them. You can fill in the blank. Bad? Hard? Absurdly bad? Absurdly hard? Mark is coming home. I feel like I should be preparing. And I am, to the best of my ability. In between bouts of lying in bed and staring out the window, trying to figure it all out.
I hit the emotional wall this week. I feel like I often try to write honestly about being a caregiver. I feel like I often fail. There are too many dimensions to caregiving. To caregiving Mark.
Part of this is because in order to survive this mammoth life curve ball, I spin my mind until I find a positive about a day, a moment, a time period. Part of this is also just my disposition. And of course there are the quiet joys. Yes, I truly can feel content when Mark and I sit in silence, watching the sparrows nesting on our porch.
As I write, I hold an acute awareness that what and how I write affects our family, friends, colleagues and community whose hearts can get beaten down with the tragedy of Mark’s circumstances, and mine, and the kids’. If you can believe this, I quite often dial back the harshness of the situation in my writing. If horror seeps through, it’s likely more horrible that I am even saying. Because everyone, including me, feels better if I’m handling it okay.
But today, I’m at a low. And I’m going to write this post for me.
Next week effectively ends what has been the most significant time in my professional life. Roughly 12 years ago, with my freshly acquired M.Ed., I responded to a newspaper ad and was hired to be a Lower School science teacher at The Ellis School. As a product of public, co-ed education, I was walking into a world that was completely new to me: a small, all-girls, PK-12 independent school. The things I noticed from day one are the things that have stood true throughout the years. People care about each other. The students are seen, known, and loved. The school values community and honors the individual. Each student and faculty member is welcomed to be who they are, to grow and shine in their interests, talents, and passions. We are colleagues and friends who love to laugh and learn together.
Over time, I moved into teaching 7th and 8th grade science and became the science department chair. I’ve been challenged and supported in becoming the best science teacher I can be. It’s a work in progress. I would never be finished. In my times of personal challenges, the staff, administration and faculty have gone many steps beyond good wishes. They have shown up. Meals, gift cards, texts, phone calls, emails. Covering my classes when Mark’s medical appointments endlessly popped up. Sitting in my empty classroom and crying with me when it was all too much.
I can’t do it anymore. I can’t take care of Mark and continue to live this part of myself. Part of this is utter exhaustion. That is not the major part. The major part is that Mark needs full time care, and my job pays less that a full-time caregiver costs. The equation is simple. Mark cannot be left alone. Period. And we’d be losing money by my working. The logic is clear and devastating.
The school, with their unrelenting kindness, is giving me a one-year leave. I don’t know if in a year my circumstances could be any different. If they are, and I can figure out a way, I will go running back to my job with open arms.
Today I toured an assisted living facility for Mark. I looked at personal care and memory units. I don’t know what will happen next with Mark. I don’t know the condition he will be in when the rehab — or insurance — decides he’s maxed out on improvements there. This morning, in an absurd moment of irony, I watched Mark pull velcroed cards off a wall, trying to arrange the letters of the alphabet from A to Z. He argued with the occupational therapist that the “I” was an “H.” He skipped the “O” and went right to the “P.”
After next week, I will no longer be a science teacher. I only will be a caregiver. Every blessing in the world of that privilege does not outweigh the reality of it. It’s an erasure of a huge part of myself, following an erasure of so many other parts of myself over the past two years. The who I knew myself to be, the highs and lows of living, all the complexities. All the freedoms.
You will want to fix this. And I appreciate that. I want to fix it, too.
I can’t figure out a way.

When I arrived on Friday morning, Mark was locked inside his bed-cage, naked except for underwear, wild-eyed and yelling at the sitter who he was convinced was employed by his former company to keep him entrapped. “Diane!” he yelled, his voice ripped with anger. “How are you doing, Mark?” I asked calmly. “I’M BEING KEPT HERE BY THIS IDIOT RPCO JERK,” he yelled, pointing at the quiet young woman sitting in a chair. RPCO was a department at Bettis that he worked in. “Can I let him out?” I asked the sitter. She said yes. I unzipped the side of the bed tent. He was naked because he was refusing to wear hospital clothes. The sitter and I helped him get into street clothes I had brought, all the while with him protesting our help. I could see that his leg drains were still intact, thankfully. Overnight, he had pulled out the top four staples from his neck. There’s nine more still in place.
Within a couple minutes, the occupational therapist, accompanied by two support people, arrived for Mark’s first therapy of the day. He was having none of it.
“What’s your name?” the OT asked him.
“COULD BE ANYTHING FROM ADAM TO ZACHARIAH!” he yelled back.
“Okay,” she said calmly. “Who is this with you?” she pointed at me.
“COULD BE ANYONE FROM ALICE TO ZEPHARELDA!”
“How many kids do you have,” she tried.
“COULD BE ANYTHING FROM 0 TO 500!” he roared.
I looked at the OT. This is a new one, I said, bewildered. He’s never done these extremes.
He did an excellent job of continuing to refuse treatment by creatively using words that began with an A and a Z. The sitter’s name could have been Aardvark or Zebra. The road we live on could be Annapolis or Zelopolopolis. “Drive,” he added to that one after a beat.
He did the same routine with speech therapy.
By the time PT came in, he had worn himself out enough that while still being belligerent, he at least complied with taking a walk. This took three staff people: two PTs on either side, and the sitter following right behind with a wheelchair in case Mark collapsed. I trailed along to watch. Mark is basically relearning how to walk.
After the therapies, I asked Mark if he wanted to look out his window with me. He paddled his wheelchair over. Mercy Hospital sits high on a hill. Mark’s corner room faces east/southeast and has a spectacular view of the Mon River, the Southside Flats and the Southside Slopes. There’s a lot to watch. Road traffic, coal barges, and kayakers. Freight trains and plane contrails. The mountainside is lush, the bridges are beautiful. If it was a hotel room, it would be thrilling.
We talked about the things we were seeing. We talked about Kennywood. He persisted in thinking he was being trapped at work, and specifically in a two year placement in Newport News, Virginia, which he really had taken in the early 2000’s. He kept asking me who was in the office. He referred to the rehab staff as “upper level administration.” I’m writing this on Sunday morning, and Mark still thinks I’m commuting five hours back and forth from Pittsburgh everyday to see him. It took me a whole day to figure out that part of his confusion about where he is is that the second window in his room overlooks construction of a new hospital building. He thinks it’s the shipyard. He points out where new fuel cell equipment is being built. Sometimes, if it feels like he is not as agitated, I remind him we are in Pittsburgh in a rehab hospital. “I keep getting confused,” he says. It’s okay, I reply. You’ll get better.
And then without warning, he will switch back to the shipyard. Back to agitation. “Where are my shoes?! Give me my shoes! These idiots are keeping them from me!”
This is the nature of Mark’s frontal lobe injury. His personality swings, he is impulsive, he is not himself. And then he is. And then again gone. He’s refusing to take meds from the nurse, because “I’m not taking anything from Newport News!” I can calmly say, hey Mark, it’s time for me to give you your meds. He will take them from me. Sometimes only after I verify that I did not get the meds from Newport News.
It’s all very disturbing, and I mean to him and to me. I can see, in his state, how he is feeling like he’s been tricked. Why he feels trapped. He is constantly being watched. He is being given tests and he can’t fully understand why or the results. He is in a locked unit and cannot get out.
At the heart of it, he is deeply confused. He is deeply afraid. And he just wants to go home.
I have no news on when that will be. The rehab staff are still getting to know him and working on a treatment plan. Everyday I go in not knowing what it will be like. I am not confused. I am a little afraid. And I am deeply exhausted.
This is how Mark’s behavior is categorized at the change of any shift. To the new nurse, the new sitter, the new nurse’s aide. “He has intermittent agitation.” This reminds me of teacher-speak for when you try to carefully explain to a parent that a kid is having a hard time. For Mark, it’s code for “keep your eyes on this one. It can come out of nowhere and be intense.”
Still, over the last couple days, they’ve been able to remove Mark’s mitts (the ones that look like boxing gloves) while keeping the “soft restraints” on. These include a vest which is strapped to the bed and canvas ties that are on 3/4 of his limbs (the doctors would not allow his incised leg to be tied down, for obvious reasons). He’s had greater periods of calm and rest. And then sometimes, something switches in his brain and the fight or flight response kicks in.
Last night, Mark was moved to what is actually the third hospital he’s be in since his surgery. His surgery was at Presby, his ICU step-down unit was in Montefiore (attached by sky bridge to Presby), and last night he was moved to a traumatic brain injury rehab unit at Mercy Hospital. Each one of these changes, for the delirium-minded patient like Mark, creates a resurgence of confusion and agitation. He will need a few days, most likely, to return to the baseline he left behind at Montefiore. And then hopefully he will climb up from there. Because as he is, there’s no way I could handle him at home.
I tried to go visit Mark at Mercy last night, but the ambulance transport turned out to be three hours late. That landed him at the new hospital after visiting hours. I drove home. A couple hours laters, we talked by phone. He was, I would say in teacher-speak, “activated.” “These people are morons!” he yelled. “They are making me stay at Bettis all night!” “I’m leaving at 3am!” You’ll have PT tomorrow, I said, to help you get stronger so you can be safe when you come home. “I’m not doing it!” he roared.
The nurse called me an hour later. They already had called security to come talk to him once. They legally cannot restrain him in the same way they can outside of a rehab unit. So now, he is in no direct restraints. Instead, they have him in the completely-ridiculously-named “canopy bed.” This is like a mesh tent they put over and attach to the bed. So, like a cloth cage. He’s unrestrained in there, but he at least can’t get out of bed which at this point with his tiny legs and buckling knees, would be devastating. I told the nurse that the chance he’ll pull out his leg drains is probably about 100%. “He’s already been going after them,” she said.
He did get one staple out of his neck already.
Last night I had a dream that I was driving a car in the dark. All of a sudden it felt like the car was driving on Vaseline. I couldn’t see anything as I slid and slid. I could hear the car going off the road, hitting brush, before finally coming to a stop in the woods.
I was not injured.
I was also not fine.
We are at rock bottom. Mark is delirious. Not the funny kind, although his wry wit still pops out from time to time. He’s hallucinating. He’s disoriented. He’s agitated. He’s worse than I have ever seen him. It’s utterly fatiguing and extremely sad.
The surgeons insist on not sedating Mark unless absolutely necessary, as they continue to manage the precarious healing from this surgery. Even with a 24/7 room sitter, Mark is battling for escape. He is wired. Perseverating on getting everything off of him. Yesterday, it took two to four of us to manage him, trying to distract him and prevent him from hurting himself. He is surprisingly fast, flexible, and strong. He was physically fighting us 90% of time that I was visiting. For all that he sleeps at home, I can not believe he is not sleeping more. For all that he sits at home, I can not believe that he can find this kind of power. As he was struggling to sit up for the nth time, the aide said, “You must have a six pack, Mark, with all this abs work you’re doing!” Mark, mishearing, replied, “I have so many odds, I’m even!” And kept fighting her to get up. Earlier in the day, he kicked an aide in the head, leading to his last free body parts, his legs, to be restrained. He tried to bite his mitts off. He wrapped his legs together and managed to pop off a drain bulb, spraying the aide with blood. She was incredibly steady and said, “You got your blood on me, Mark, that’s not nice.” He looked at her, wild-eyed, and said, “Hehehehehe!” I said, “Use your power for good, Mark,” and he cried back, “Evil!” He was out of his freakin’ mind. He kept calling out for help. He kept telling nurses he was being picked on. He told us that he was going to take us to court, and that the judge would put us in jail for six months for what we were doing to him.
I am numb and feel like I am running a daily physical marathon. My muscles are tired. I have only one focus, and that’s to keep going. It’s ugly right now. Keep going…keep going…keep going….
When I checked into the hospital today, the staff person put my visitor’s bracelet on my wrist and said, “This gets you half-off drinks during happy hour. All the rides are running, and the swimming pool is open.” It took me a minute to open up my thinking to process the quiet humor. “That’s good,” I replied, “I can go there in my mind.” “Good,” he said, and waved me through to live another day just like yesterday.


